Boston Children’s Hospital History
1869-1881
Soon after the Civil War, in 1869, Dr. Francis Henry Brown organized a small group of Harvard Medical School graduates joined by Boston’s civic leaders to establish a 20 bed Children’s Hospital in a townhouse on Rutland Street in Boston’s South End. The hospital treated just 30 patients that first year. One year later the Children’s Hospital relocated to a larger building on the same street. The patients were predominately Irish immigrants and many had traumatic injuries or infectious diseases. Philanthropy completely supported the new hospital. Sister Theresa and the Anglican Order of the Sisters of St. Margaret oversaw the nursing care of the children for the first 45 years of the hospital’s existence.
1892-1913
By 1882 having outgrown its current structure, the hospital was moved to Huntington Avenue near the current Symphony Hall. This larger building was designed especially for children’s needs. As the range of illnesses grew, so did the professional staff. Between the years 1882 and 1914 the practice of pediatrics was recognized as a specialty and Harvard Medical School made its first appointment of a physician devoted solely to the care of children. The first medical house officers (interns and externs) were appointed and a nursing school was opened to educate nurses. Children’s Hospital’s neighbors were far different in 1914 than today.
1914-1945

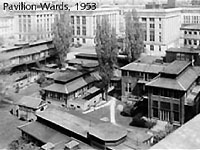
In the early 1900s Harvard Medical School moved to the former Ebenezer Francis Farm, its current site, and in 1914 the Children’s Hospital relocated to its current address on Longwood Avenue immediately adjacent to the Medical School. During this era the Hunnewell building housed the children until a series of “cottages” were built in an effort to prevent the spread of infection. These “cottages” housed medical, surgical and orthopedic patients. Departments now differentiated into Surgery, Medicine, Radiology, Orthopaedics, and Pathology to mention only a few. Cystic fibrosis, erythroblastosis fetalis and other diseases were described and studied. Pediatric medicine subspecialized into metabolism, hematology and bacteriology. Surgeons developed new techniques for repairing congenital abnormalities. The field of cardiac surgery was begun and the iron lung for polio victims was developed by physicians at Children’s Hospital and the Harvard School of Public Health. Harvard medical students began to learn pediatrics at the Children’s Hospital. The housestaff grew from 3-4 in 1900 to over 30 in the early 40s. Women became residents when men left to serve in World War II. The Medical & Nursing Alumni Associations were established. During this period, Children’s Hospital forged strong bonds with other institutions including the House of the Good Samaritan (for rheumatic fever patients), the Sarah Fuller School (for deaf children), the Judge Baker Children’s Center (for psychiatric illness) and the Sharon Sanatorium. Remarkably, in 1939 the average cost of a hospital visit was just $1.50.
1946-1990
During the years 1946 to 1990 the Children’s Hospital was well positioned to take a leadership role in pediatric health. Experienced physicians returned from the military service. The NIH established programs to support academic research. The Children’s Hospital organized itself into the Children’s Hospital Medical Center. The hospital endorsed specialized pediatric care, and began the construction of new buildings: the Farley inpatient building (in 1956), the Fegan outpatient building (in 1967), the Martha Eliot Health Center (in 1967), and the Enders research building (1970) named for Dr. John Enders, recipient of the Nobel Prize for his work with polio virus. In1987 a new inpatient facility was built bringing the number of inpatient beds to 330. Old diseases such as polio, measles, pertussis, meningitis, pneumonias, and epiglottitis decreased in prevalence because of vaccines, and new antibiotics, only to be replaced by new diseases like HIV, Kawasaki’s, substance abuse, and the autism spectrum disorders. The faculty in all departments grew rapidly. The medical housestaff by 1990 numbered over 86 residents. All subspecialties had developed outstanding fellowships. The hospital was now a primary education site for Harvard medical students and elective students from throughout the US, and Children’s Hospital enjoyed both a national and international reputation.
1990-Present

The years since 1990 have seen increasing excellence in patient care, great research productivity, new medical innovations, and remarkable contributions to pediatric medical education. Children’s Hospital clinicians have pioneered lung, liver, and multiple organ transplants, innovative procedures for short gut syndrome, surgery using robotics and lasers, the development of tissue engineered organs, the use of small devices to repair holes in the heart, hydroxyurea to treat sickle cell disease, gene therapy, novel treatments for vascular malformations, and fetal intervention for hypoplastic left heart syndrome, among others. Children’s researchers have developed treatments for blood disorders, regenerated damaged nerves, identified genes associated with specific diseases, developed new vaccines for serious illnesses, created disease-specific human stem cells, invented genomic tools to classify tumors and identify new drug therapies, and developed whole new fields, such as angiogenesis.



